Diseases & Conditions
Stress Fractures of the Foot and Ankle
A stress fracture is a small crack in a bone, or severe bruising within a bone. Most stress fractures are caused by overuse and repetitive activity; they are common in runners and athletes who participate in running-intensive sports, such as soccer and basketball.
Pain from stress fractures usually develops gradually and is worse during weight-bearing activities. You also typically experience point tenderness at the site of the fracture.
Stress fractures sometimes occur when people change their activities — such as trying a new exercise, suddenly increasing the intensity of their workouts, or changing workout surfaces (jogging on a treadmill vs. jogging outdoors). In addition, if osteoporosis or other disease has weakened the bones, just doing everyday activities may result in a stress fracture.
The weight-bearing bones of the foot and lower leg are especially vulnerable to stress fractures because of the repetitive forces they must absorb during activities like walking, running, and jumping.
Temporarily refraining from high impact activities is key to recovering from a stress fracture in the foot or ankle. Returning to activity too quickly can not only delay the healing process but also increase the risk of a complete fracture. Should a complete fracture occur, it will take far longer to recover and return to activities.
Description
Many stress fractures are overuse injuries. They occur over time when repetitive forces result in microscopic damage to the bone. The repetitive force that causes a stress fracture is not great enough to cause an acute fracture — such as a broken leg caused by a fall or crash. Overuse stress fractures occur when an athletic movement is repeated so often that weight-bearing bones and support muscles do not have enough time to heal between exercise sessions.
Bone is in a constant state of turnover — a process called remodeling. New bone develops and replaces older bone. With too much activity, the breakdown of older bone can occur rapidly and outpaces the body's ability to repair and replace it. As a result, the bone weakens and becomes vulnerable to stress fractures.
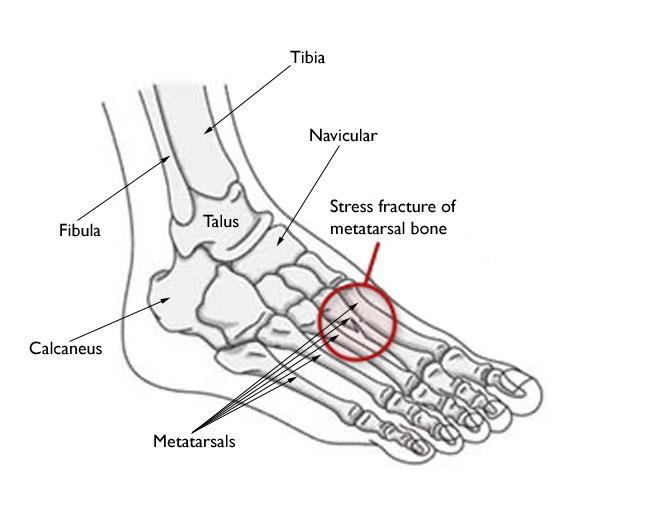
Stress fractures in the foot and ankle occur are most common in the metatarsal bones. They are also often seen in the calcaneus (heel); fibula (the outer bone of the lower leg and ankle); talus (the lower bone in the ankle joint); sesamoids (two small bones associated with the tendons of the big toe; and the navicular (a bone on the top of the midfoot).
Stress Fractures of the Metatarsal Bones
The second and third metatarsals of the foot, which are thinner (and often longer) than the adjacent first metatarsal, are most prone to stress fractures. This is the area of greatest impact on your foot when you push off to walk or run. Therefore, ballet dancers are at particularly high risk of developing these injuries. People who have a larger second metatarsal bone are also at risk. These fractures typically cause generalized pain in the middle of the foot.
Less commonly, people may have fractures of the fourth and fifth metatarsals, causing pain on the outside of the foot. These fractures can occasionally be more difficult to treat, as some areas of these bones (specifically, the base of the fifth metatarsal) do not receive a large blood supply, which leads to longer healing times.
Stress Fractures of the Fifth Metatarsal Base
Stress fractures at the base of the fifth metatarsal deserve special attention. This injury was first described by Sir Robert Jones in the early 1900s, and since then the injury has often been referred to as a Jones fracture. This injury may present itself as the onset of pain on the outside of the midfoot, often without acute injury. It is particularly common in high-level athletes.
Stress fractures of the fifth metatarsal base are challenging to treat because the body's blood supply to this area is poor and, therefore, healing takes longer.
Nonsurgical management typically consists of non-weightbearing immobilization (cast or boot) for at least 6 weeks. Your physician may prescribe vitamin D, a bone stimulator, or other methods to increase the healing potential. You are usually not able to return to sports until 12 weeks post-injury.
In some cases — for instance, if you are a high-level athlete — your doctor may speak to you about surgical options to stabilize the bone and increase the healing potential. Surgery may involve placement of a screw, bone grafting, or a combination or plates and screws. To obtain the best outcome, it is very important to follow the post-surgical activity restrictions that your doctor recommends.
Learn more: Toe and Forefoot Fractures
Stress Fractures of the Calcaneus (Heel Bone)
The calcaneus is the bone that makes up the heel of your foot. It is the second most common area of the foot to develop stress fractures. If often presents as pain in the heel occurring with exercise. This discomfort can be similar to the discomfort caused by plantar fasciitis (inflammation of the connective tissue on the sole of your foot) or bone spurs of the heel. Therefore, your doctor may recommend an MRI scan to help make the diagnosis.
Learn more: Calcaneus (Heel Bone) Fractures
Stress Fractures of the Navicular
The navicular is one of the bones in the middle of the foot. Stress fractures of the navicular cause pain that is difficult to pinpoint. The pain is worsened by weightbearing and other physical activities, such as sprinting or jumping. The navicular bone is not commonly associated with stress fractures, and the diagnosis can sometimes be hard to make. Your doctor may order a CT scan or MRI scan if they are concerned that you have a navicular stress fracture.
Treatment of this injury can sometimes require a cast and a period of non-weightbearing for a few weeks. This is one type of stress fracture where surgery is more commonly recommended to stabilize the bones and expedite healing.
Stress Fracture of the Talus
The talus is one of the bones in the heel of the foot. It is an uncommon bone to be affected by stress fracture. When it does occur, however, it can cause pain in the heel or ankle.
Stress Fracture of the Sesamoids
The sesamoids are two small bones located in the ball of the foot, beneath the joint of the big toe. These bones act as a pulley for the muscles that power the big toe and help it move normally when walking and running. These small bones can sometimes be affected by stress fractures. If this occurs, you will experience pain in the foot around the base of the big toe. Diagnosis can be hard to make on X-rays; therefore, your doctor may order an MRI or bone scan if they suspect a stress fracture.
Cause
The most common cause of stress fractures is a sudden increase in physical activity. This increase can be in the frequency of activity — such as exercising more days per week. It can also be in the duration or intensity of activity — such as running longer distances or repetitive high-impact activities following weight gain.
Even for the non-athlete, a sudden increase in activity can cause a stress fracture. For example, if you walk infrequently on a day-to-day basis but end up walking excessively (or on uneven surfaces) while on a vacation, you might experience a stress fracture. And a new style of shoes can lessen your foot's ability to absorb repetitive forces and result in a stress fracture.
Bone Insufficiency
Certain long-term medications or conditions that cause a decrease in bone strength, such as osteoporosis, can make you more likely to experience a stress fracture even when you are performing normal everyday activities. For example, stress fractures are more common in the winter months, when Vitamin D is lower in the body.
Studies show that female athletes are more prone to stress fractures than male athletes. This may be due, in part, to decreased bone density from a condition that doctors call the "female athlete triad." When a girl or young woman goes to extremes in dieting or exercise, three interrelated illnesses may develop: eating disorders, menstrual dysfunction, and premature osteoporosis. As a female athlete's bone mass decreases, her chances for getting a stress fracture increase.
Poor Conditioning
Doing "too much, too soon" is a common cause of stress fracture. This is often the case with individuals who are just beginning an exercise program, but it occurs in experienced athletes as well. For example, runners who train less over the winter months may be anxious to pick up right where they left off at the end of the previous season. Instead of starting off slowly, they resume running at their previous mileage. This situation, in which athletes increase activity levels, push through significant discomfort, and do not give their bodies the opportunity to recover, can lead to stress fractures.
Improper Technique
Anything that alters the mechanics of how your foot absorbs impact as it strikes the ground may increase your risk for a stress fracture. For example, if you have a blister, bunion, or tendonitis, it can affect how you put weight on your foot when you walk or run. This may alter your weightbearing mechanics, leading to more weight and pressure than usual on certain bones.
Change in Surface
A change in training or playing surface, such as a tennis player going from a grass court to a hard court, or a runner moving from a treadmill to an outdoor track, can increase the risk for stress fracture.
Improper Equipment
Wearing worn or flimsy shoes that have lost their shock-absorbing ability may contribute to stress fractures.
Symptoms
The most common symptom of a stress fracture in the foot or ankle is pain. The pain usually develops gradually and worsens during weight-bearing activity. Other symptoms may include:
- Pain that diminishes during rest
- Pain that is associated with physical activities throughout the day
- Swelling on the top of the foot or on the outside of the ankle
- Tenderness to touch at the site of the fracture
- Possible bruising
First Aid
See your doctor as soon as possible if you think that you have a stress fracture in your foot or ankle. Ignoring the pain can have serious consequences. The bone may break completely.
Until your appointment with the doctor, follow the RICE protocol. RICE stands for rest, ice, compression, and elevation.
- Rest. Avoid activities that put weight on your foot. If you must bear weight for any reason, make sure you are wearing a very supportive shoe. A thick-soled cork sandal is better than a thin slipper. Make sure to listen to your body. If certain positions or activities are making your pain worse, that is your body telling you that you are putting stress on the injury site.
- Ice. Apply ice immediately after the injury to keep the swelling down. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly on your skin.
- Compression. To prevent additional swelling, lightly wrap the area in a soft bandage.
- Elevation. As often as possible, rest with your foot raised up higher than your heart.
In addition, nonsteroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen or naproxen can help relieve pain and reduce swelling.
Doctor Examination
Physical Examination
Your doctor will discuss your medical history and general health. They will ask about your work, your activities, your diet, and what medications you are taking. It is important that your doctor is aware of your risk factors for stress fracture. If you have had a stress fracture before, your doctor may order a full medical work-up with laboratory tests to check for nutritional deficiencies such as low calcium or Vitamin D.
After discussing your symptoms and health history, your doctor will examine your foot and ankle. During the examination, they will look for areas of tenderness and apply gentle pressure directly to the injured bone. Often, the key to diagnosing a stress fracture is the patient's report of pain in response to this pressure. Pain from a stress fracture is typically limited to the area directly over the injured bone and is not generalized over the whole foot.
Imaging Tests
Your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Since a stress fracture starts as a tiny crack, it is often difficult to see on a first X-ray. The fracture may not be visible until several weeks later when it has started to heal. After a few weeks, a type of healing bone called callus may appear around the fracture site. In many cases, this is the point at which the fracture line becomes visible in the bone.
Other imaging tests. If your doctor suspects a stress fracture but cannot see it on an X-ray, they may recommend a bone scan or a magnetic resonance imaging (MRI) scan. Although a bone scan is less specific than an MRI in showing the actual location of the stress fracture, both types of studies are more sensitive than X-rays and can detect stress fractures earlier.
If your stress fracture occurred with light activity, your doctor may recommend a bone density scan (DEXA scan) to look at the strength of your bones overall. This can be helpful in diagnosing osteoporosis, and the results of this test can help your doctor determine whether you are a candidate for medications to help strengthen your bones.
Treatment
The goal of treatment is to relieve pain and allow the fracture to heal so you can return to your activities. Following your doctor's treatment plan will help you return to activities faster and prevent further damage to the bone.
Treatment will vary depending on the location of the stress fracture and its severity. Most stress fractures are treated nonsurgically.
Nonsurgical Treatment
In addition to the RICE protocol and anti-inflammatory medication, your doctor may recommend that you use crutches to keep weight off your foot until the pain subsides. Other recommendations for nonsurgical treatment may include:
Modified activities. It typically takes 6 to 8 weeks for a stress fracture to heal. During that time, switch to activities that place less stress on your foot and leg. Swimming and cycling are good alternative activities. However, you should not resume any type of physical activity that involves your injured foot or ankle — even if it is low impact — without your doctor's approval.
Protective footwear. To reduce stress on your foot and leg, your doctor may recommend wearing protective footwear. This may be a stiff-soled shoe, a wooden-soled sandal, or a removable short-leg fracture brace shoe.
Casting. Certain types of stress fractures may require additional stability. Your doctor may apply a cast to your foot to keep your bones in a fixed position and remove the stress on your involved leg.
Surgical Treatment
Some stress fractures require surgery to heal properly. In most cases, this involves supporting the bones by inserting a type of internal fixation. Specialized pins, screws, and/or plates are most often used to hold the small bones of the foot and ankle together during the healing process. Surgery may also be needed if a stress fracture breaks completely and displaces.
Your surgeon may perform this type of surgery by either making a small incision near the fractured bone or by inserting pins/screws through the skin. Most of the time, the hardware does not need to be removed after the bone has healed. Occasionally, however, your surgeon may advise removal of the hardware; this is typically a quick outpatient procedure.
Recovery
In most cases, it takes 6 to 8 weeks for a stress fracture to heal. More serious stress fractures can take longer. Chronic stress fractures or stress fractures in bone with less blood supply can take longer to heal.
Although it can be hard to be sidelined with an injury, returning to activity too soon can put you at risk for prolonged recovery or even a sudden worsening of the fracture that could require surgery.
Once your pain has subsided, your doctor may confirm that the stress fracture has healed by taking X-rays. A computed tomography (CT) scan can also be useful in determining healing, especially in bones where the fracture line was initially hard to see.
Once the stress fracture has healed and you are pain-free, your doctor will allow a gradual return to activity. During the early phase of rehabilitation, your doctor may recommend alternating days of activity with days of rest. This gives your bone time to grow and withstand the new demands being placed upon it. As your fitness level improves, you can slowly increase the frequency, duration, and intensity of your exercise.
Prevention
The following guidelines can help you prevent stress fractures in the future:
- Eat a healthy diet. A balanced diet rich in calcium and Vitamin D will help build bone strength.
- Use proper equipment. Old or worn running shoes may lose their ability to absorb shock and can lead to injury. In general, athletic shoes should have a softer insole, and a stiffer outer sole. Learn more: Athletic Shoes
- Start new activity slowly. Gradually increase your time, speed, and distance. In most cases, a 10% increase per week is appropriate.
- Cross train. Vary your activities to help avoid overstressing one area of your body. For example, alternate a high-impact sport like running with lower-impact sports like swimming or cycling.
- Add strength training to your workout. One of the best ways to prevent early muscle fatigue and the loss of bone density that comes with aging is to incorporate strength training. Strength-training exercises use resistance methods like free weights, resistance bands, or your own body weight to build muscles and strength.
- Stop your activity if pain or swelling returns. Rest for a few days. If the pain continues, see your doctor.
Last Reviewed
March 2022
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.