Diseases & Conditions
Pigmented Villonodular Synovitis
Pigmented villonodular synovitis (PVNS) is a condition that causes the synovium—the thin layer of tissue that lines the joints and tendons—to thicken and overgrow. The mass or tumor that results from this overgrowth is not cancerous and does not spread (metastasize) to other areas of the body. However, PVNS is a progressive disease. It slowly worsens and can lead to bone damage and arthritis.
PVNS usually affects the knee, although it can affect other joints as well. In most cases, surgery is needed to remove the damaged joint lining and the mass.
Description
In a healthy joint, the synovium produces a small amount of fluid that lubricates the cartilage and aids in movement. In PVNS, the synovium produces extra fluid, causing swelling in the joint and making movement very painful.
PVNS typically involves only one joint. In 80% of patients, the knee is involved, but PVNS can also affect the hip, ankle, shoulder, and elbow. The condition can affect people of all ages, but it occurs most often in young adults from 20 to 50 years of age.
There are two forms of PVNS—localized and diffuse.
Localized PVNS
When the tumor involves the tendons that support the joint, or occurs in just one area of the joint, it is called localized PVNS. This type usually responds well to treatment.
Diffuse PVNS
When the condition is more widespread and involves an entire joint, it is called diffuse PVNS. It tends to be more aggressive and is more difficult to treat.
Cause
The cause of PVNS is not known. Genetic changes associated with PVNS have been identified, but the evidence for a genetic cause is not clear at this time.
In some patients with PVNS, a small number of cells in the lining of the affected joint have a defect that makes them produce a protein called colony-stimulating factor 1 receptor (CSF-1R). Research has shown that this protein is involved in PVNS.
Symptoms
Localized PVNS causes pain and swelling in the affected joint. The swelling can be quite significant. Other symptoms may include locking, catching, and instability in the joint.
In diffuse PVNS, there is often a gradual onset of symptoms including joint pain, swelling, and stiffness. Sometimes, patients may present with hemarthrosis, a condition in which blood collects in the joint space. This can occur with minimal or even no trauma to the affected joint.
In both types, the symptoms may come and go over time.
Doctor Examination
Your doctor will perform a physical examination and use imaging studies and other tests to diagnose PVNS.
Tests
X-rays. X-rays provide clear pictures of dense structures, such as bone. If PVNS has not damaged or caused changes in your bone, it may not appear in an x-ray. However, x-ray images may help your doctor rule out other causes for your pain.
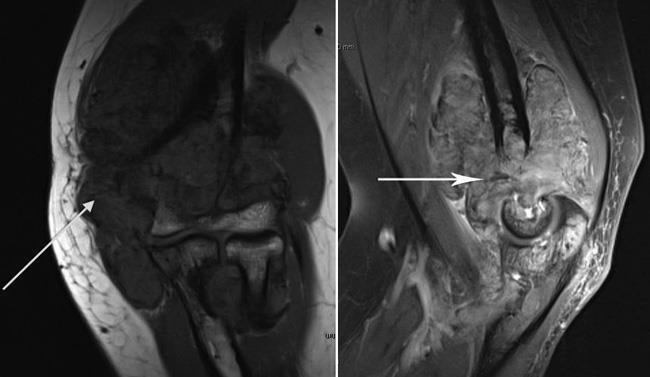
Magnetic resonance imaging (MRI) scan. An MRI provides clear images of the body's soft tissues and can be helpful in diagnosing PVNS. In localized PVNS, an MRI will show a nodular mass. In diffuse PVNS, it will show extensive thickening of the joint lining or an extensive mass, possibly with destructive bone changes and cartilage damage.
Joint aspiration. In this procedure, fluid is removed from the joint with a syringe and analyzed. In many cases of PVNS, the joint fluid is bloody.
Biopsy. A biopsy may be necessary to confirm the diagnosis of PVNS. In a biopsy, a tissue sample of the tumor is taken and examined under a microscope. A small operation is required to obtain a tissue sample.
Treatment
Because PVNS destroys healthy bone and can grow to a large size, treatment typically involves surgery to remove the tumor and the damaged portions of the joint lining. When localized PVNS has also damaged a tendon, your surgeon will repair it during the procedure to remove the tumor. Your doctor will discuss the various surgical options with you.
Surgical Procedures
Arthroscopy. In many cases of both localized and diffuse PVNS, the tumor and damaged joint lining are removed arthroscopically.
During arthroscopy the surgeon makes a few small incisions around the joint and inserts a small camera called an arthroscope. The camera displays pictures on a video monitor, and the surgeon uses these images to guide miniature surgical instruments.
Open surgery. Diffuse PVNS that affects both the front and back of the knee requires removal of the entire joint lining to reduce the chances of the tumor returning. In many cases, this is best achieved with traditional "open" surgery. A single larger incision provides the surgeon with full access to the joint, and facilitates removal of the mass and the entire joint lining.
Combined arthroscopic and open surgery. When most of the mass is in the back of the knee, a combined surgical approach can be undertaken. The back of the knee is treated with open surgery to remove the mass and posterior joint lining, and the front of the knee is treated with arthroscopic removal of the anterior joint lining. This combined method decreases the scale of surgery, allowing for an easier recovery.
Total joint replacement. In its end stages, diffuse PVNS can cause extensive joint destruction. Once the joint has been significantly damaged, the best option to relieve pain and improve function is a total joint replacement. Total joint replacement is a procedure in which parts of a damaged joint are removed and replaced with metal, plastic, or ceramic components. In some cases, the tumor may return even after the joint has been replaced.
Radiation
Radiation therapy can shrink tumors and is sometimes used to treat widespread diffuse PVNS. It is usually reserved for patients in whom standard surgery has not been successful.
In the past, radiation therapy has been given via an external beam that is directed from outside the skin to the inside of the affected joint. While often successful, this method can cause complications.
A newer method called intra-articular radiation has also been used successfully. During this procedure, radioactive fluid is injected into the joint with a needle.
For some patients, radiation therapy may be used after surgery to lower the recurrence risk.
Drug Therapy
There are currently several medications being studied for the treatment of PVNS. These medications specifically target the CSF-1R protein produced by cells in the joint lining and have been shown to be effective in some patients. Your doctor will talk with you about whether you are a good candidate for drug therapy.
Recovery
After surgery, physical therapy will be extremely important in helping you return to your daily activities. Specific exercises will help you regain strength and range of motion in the affected joint.
Recovery from arthroscopic surgery usually requires a short course of physical therapy, after which you may return to normal activity.
Open surgery is more extensive, however, so there is an increased risk of postoperative stiffness. A more regimented and extensive physical therapy program is often required for patients recovering from open surgery to treat diffuse PVNS. In this case, the return to normal activity will take longer—possibly several months.
Localized PVNS rarely recurs after surgery. The recurrence rate for diffuse PVNS is usually around 10%, but can be as high as 30%. Patients with diffuse PVNS will require physician follow-up for several years after surgery. During these visits your doctor may order tests such as an MRI to check for recurrence of PVNS.
Last Reviewed
May 2020
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.