Diseases & Conditions
Achilles Tendinitis
Achilles tendinitis is a common condition that occurs when the large tendon that runs down the back of the lower leg becomes irritated and inflamed.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone and is used when you walk, run, climb stairs, jump, and stand on your tip toes. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse.
Description
Simply defined, tendinitis (also spelled "tendonitis") is acute inflammation of a tendon. Inflammation is the body's natural response to injury and often causes swelling, pain, or irritation.
You may also come across the term "tendinopathy," which is used to describe a condition in which the tendon develops microscopic degeneration as a result of chronic damage over time. Tendinitis, tendinosis, and tendinopathy are all common terms which essentially refer to the same problem.
Achilles tendinitis is different than an Achilles rupture, a condition where the tendon becomes separated off the heel bone or completely torn in half. Achilles tendon rupture typically results from a sudden injury. This article will focus on Achilles tendinitis rather than Achilles tendon rupture.
There are two types of Achilles tendinitis, based on which part of the tendon is inflamed. The two types can occur separately or at the same time.
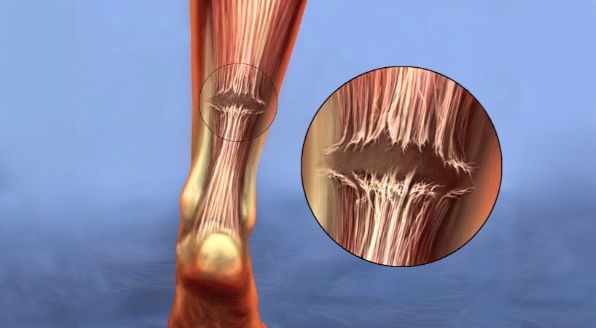
Noninsertional Achilles Tendinitis
In noninsertional Achilles tendinitis, fibers in the middle portion of the tendon (above where it attaches to the heel) are affected. Over time, the fibers may begin to break down and develop tiny tears. This can lead to tendon swelling and thickening.
Noninsertional tendinitis more commonly affects younger, active people, especially runners.
Insertional Achilles Tendinitis
Insertional Achilles tendinitis involves the lower portion of the tendon, where it attaches (inserts) to the heel bone (also known as the calcaneus).
In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may calcify (harden) over time. Bone spurs often form on the heel with insertional Achilles tendinitis.
Insertional Achilles tendinitis can occur at any time or activity level, although it is still most common in runners. It is frequently caused by calf muscle tightness, which places increased stress on the Achilles tendon insertion.
Cause
Achilles tendinitis is typically not related to a specific injury. The problem results from repetitive stress to the tendon. This often happens when we push our bodies to do too much, too quickly. Other factors can also make a person more likely to develop Achilles tendinitis, including:
- A sudden increase in the amount or intensity of exercise activity. For example, increasing the distance you run every day by a few miles without giving your body a chance to adjust to the new distance may cause irritation and inflammation.
- Tight calf muscles. Calf muscle tightness puts extra stress on the Achilles tendon, especially where it inserts into the heel bone.
- Haglund's deformity. This is a condition in which there is enlargement of the bone on the back of the heel. This can rub on the Achilles tendon and cause inflammation and pain.
Symptoms
Common symptoms of Achilles tendinitis include:
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Thickening of the tendon
- Bone spur formation (insertional tendinitis)
- Swelling that is present all the time and gets worse throughout the day or with activity
- Pain on the back of the heal when you wear shoes
If you have experienced a sudden pop in the back of your calf or heel, you may have torn your Achilles tendon. See your doctor immediately if you think you may have torn your tendon.
Doctor Examination
After you describe your symptoms and discuss your concerns, the doctor will examine your foot and ankle. The doctor will look for these signs:
- Swelling along the Achilles tendon or at the back of your heel
- Bone spurs or pain near the lower part of the tendon at the back of your heel (insertional tendinitis)
- Pain in the middle of the tendon, (noninsertional tendinitis)
- Heel pain when stretching your calf
- Limited range of motion in your ankle — specifically, a decreased ability to point your toes downward
Tests
Your doctor may order imaging tests to help determine if your symptoms are caused by Achilles tendinitis. These tests can also help your doctor ascertain the severity of your Achilles tendinitis.
X-rays
X-rays provide clear images of bones. They can show bone spurs on the back of the heel, which may be present in patients with insertional Achilles tendinitis. In cases of severe noninsertional Achilles tendinitis, X-rays may show calcification in the middle portion of the tendon.
Magnetic Resonance Imaging (MRI)
Although magnetic resonance imaging (MRI) is not necessary to diagnose Achilles tendinitis, it is important for planning surgery if nonsurgical treatment is not effective. An MRI scan can show the severity of the damage in the tendon. If surgery is needed, your doctor will select the procedure based on the amount of tendon damage.
Ultrasound
Ultrasound has grown in popularity among physicians in recent years. It is quicker and less expensive than MRI and may be readily performed in an office setting. However, ultrasound is more operator-dependent than MRI and may yield less consistent results.
Treatment
Nonsurgical Treatment
In most cases of Achilles tendinitis, nonsurgical treatment options will provide adequate pain relief, although it may take a few months for symptoms to completely subside. Even with early treatment, the pain may last longer than 3 months.
The mainstays of nonsurgical treatment include anti-inflammatory pain medications, activity modification, shoe wear modification, and physical therapy exercises.
Rest
The first step in reducing pain is to decrease or even stop the activities that make the pain worse. If you regularly participate in high-impact exercises (such as running), switching to low-impact activities will decrease the amount of stress on the Achilles tendon. Cross-training activities such as biking, elliptical exercise, and swimming are low-impact options to help you stay active. Your doctor may recommend an ankle brace or boot immobilization to help with this step.
Ice
Placing ice on the most painful area of the Achilles tendon is helpful and can be done as needed throughout the day. This can be done for up to 20 minutes at a time, but the ice should be removed sooner if the skin becomes numb.
A foam cup filled with water and then frozen creates a simple, reusable ice pack. After the water has frozen in the cup, tear off the rim of the cup. Then rub the ice on the Achilles tendon. With repeated use, a groove that fits the Achilles tendon will appear, creating a custom-fit ice pack.
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
Anti-inflammatory drugs such as ibuprofen and naproxen reduce pain and swelling. They can help decrease your pain enough to allow you to perform physical therapy exercises as discussed below. They do not, however, reduce the thickening of the degenerated tendon. Using the medication for more than 1 month should be reviewed with your primary care doctor.
Physical Therapy
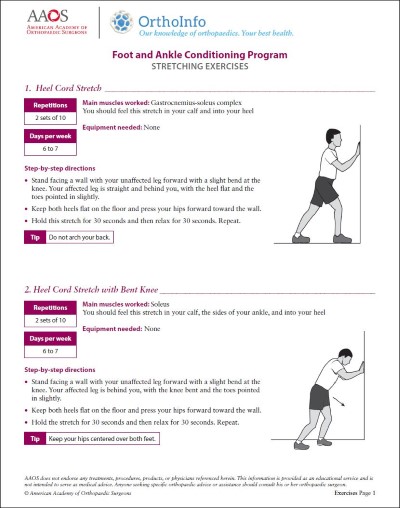
Physical therapy is very helpful in treating Achilles tendinitis. The following exercises and stretches can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
Calf stretch. Lean forward against a wall with one knee straight and your heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. You should feel a strong pull in the calf during the stretch.
Eccentric Strengthening. Eccentric strengthening is defined as contracting (tightening) a muscle while it is getting longer. Eccentric strengthening exercises can cause damage to the Achilles tendon if they are not done correctly. At first, they should be performed under the supervision of a physical therapist. Once mastered with a therapist, the exercises can then be done at home. These exercises may cause some discomfort, but it should not be unbearable:
- Bilateral heel drop
Stand at the edge of a stair, or a raised platform that is stable, with just the front half of your foot on the stair. This position will allow your heel to move up and down without hitting the stair. Care must be taken to ensure that you are balanced correctly to prevent falling and injury. Be sure to hold onto a railing to help you balance.
Lift your heels off the ground then slowly lower your heels to the lowest point possible. Repeat this step 20 times. This exercise should be done in a slow, controlled fashion. Rapid movement can create the risk of damage to the tendon. As the pain improves, you can increase the difficulty level of the exercise by holding a small weight in each hand.
- Single leg heel drop
This exercise is performed similarly to the bilateral heel drop, except that all your weight is focused on one leg. This should be done only after the bilateral heel drop has been mastered.
Cortisone Injections
Cortisone, a type of steroid, is a powerful anti-inflammatory medication. While injections can be used in other injuries and conditions, cortisone injections into the Achilles tendon are not recommended because they can cause the tendon to rupture (tear). In fact, research has shown significantly decreased tendon strength after steroid injection.
Other injectable substances, such as platelet-rich plasma (PRP) have been studied for Achilles tendinitis, and several studies on PRP injections have shown improvements in pain. However, more information is needed to determine how effective PRP truly is for this condition.
Night Splinting
Night splinting can provide significant relief for morning pain when you first get out of bed. These removable braces work by holding your foot in place with your toes pointing upward (similar to the calf stretch position) while you sleep. This helps to maintain calf flexibility and decrease the pull of your Achilles tendon on your heel.
Supportive Shoes and Orthotics
Insertional Achilles tendinitis is often relieved by certain shoes and orthotic devices. For example, shoes that are softer or open at the back of the heel can reduce irritation of the tendon. Heel lifts are another option and can decrease the amount of strain off the tendon.
If your pain is severe, your doctor may recommend a walking boot for a short time. This gives the tendon a chance to rest before initiating therapy. However, extended use of a boot is discouraged because it can weaken the calf muscle.
Extracorporeal Shockwave Therapy (ESWT)
This therapy uses either low- or high-energy shockwaves applied to the Achilles tendon to promote healing of the damaged tendon tissue.
- High-energy ESWT can be done in one visit but requires local or general anesthesia.
- Low-energy ESWT consists of 3 to 4 sessions and does not require local anesthesia.
Recent studies have shown improvement in pain and function with ESWT, especially when combined with other nonsurgical treatments such as eccentric exercises. However, more information is needed before strong recommendations can be made for its routine use. One benefit of ESWT is that it is low risk and has few to no complications, so it may be another option to consider before undergoing surgery.
Surgical Treatment
Surgery for Achilles tendinitis should be considered only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon.
Debridement
Debridement is a term that refers to the removal, or "cleaning up," of damaged tissue. For insertional Achilles tendinitis, removal of the bone spurs from the heel in addition to the damaged tendon tissue is commonly performed with good outcomes. Once the unhealthy portion of the tendon is removed, the remaining tendon can be reattached to the heel bone. Metal or plastic anchors as well as strong stitches may be placed into the heel bone to help hold the tendon in place.
After debridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although the timeline depends on the amount of damage to the tendon.
In cases where more than 50% of the Achilles tendon must be removed, the remaining portion of the tendon is not strong enough to function alone. Another tendon must be transferred in order to restore the strength to your foot for pushing off the ground. The tendon that helps the big toe flex down (the flexor halluces longus [FHL] tendon) is most commonly used. This tendon is removed from the bottom of the big toe and reattached to the heel. After this surgery, the big toe is still able to move, and most patients do not notice a change in the way they walk or run.
Gastrocnemius Recession
This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope — an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low but can include nerve damage.
Minimally Invasive Surgery
Minimally invasive surgery has been increasing in popularity for treatment of many musculoskeletal conditions. For Achilles tendinitis, it may involve using small incision to place a camera and small instruments through the skin to remove damaged and inflamed Achilles tendon tissue.
Other minimally invasive surgeries include using small holes to release parts of the tendon and muscle from the bone. These techniques may become more popular with time, but there is still limited information on their effectiveness. Additionally, they may be less effective in patients with extensive tendon damage.
Outcomes
Results of Achilles tendinitis surgery are generally very good. Studies on tendon debridement have reported return to pre-surgical activity level in up to 75% of patients, with up to a 90% patient satisfaction rate. Gastrocnemius recession has also shown good results, with high rates of reduced pain and improved function after surgery.
The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity.
Physical therapy is an important part of recovery. Many patients require up to 12 months of rehabilitation to reach maximum improvement.
Continued pain after surgery may be noted in up to 20% to 30% of patients and is the most common complication. In addition, wound infections can occur and may be difficult to treat in this location on the body.
Last Reviewed
March 2022
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.