Treatment
Unicompartmental (Partial) Knee Replacement
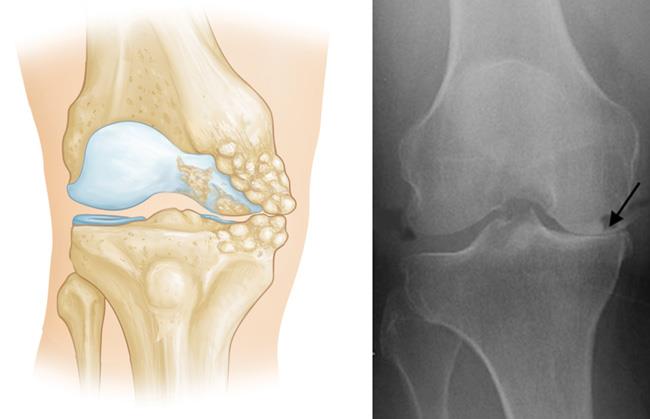
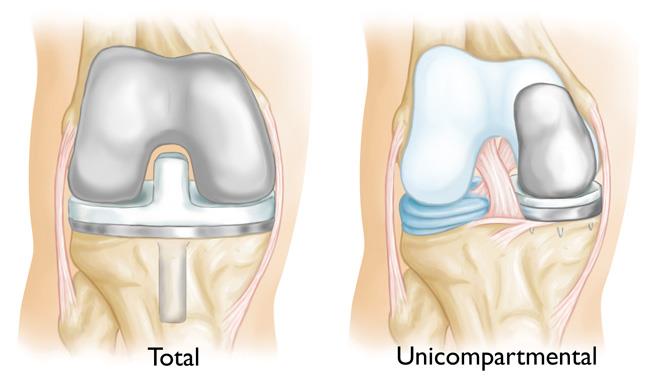
During knee replacement surgery, bone and cartilage damaged by osteoarthritis are resurfaced with metal and plastic components. In unicompartmental knee replacement (also called partial knee replacement) only a portion of the knee is resurfaced. This procedure is an alternative to total knee replacement for patients whose disease is limited to just one area of the knee.
Because a partial knee replacement is performed through a smaller incision, patients usually spend little or no time in the hospital and return to normal activities sooner than total knee replacement patients.
There are a range of treatments for knee osteoarthritis, and your doctor will discuss with you the options that will best relieve your individual osteoarthritis symptoms.
Description
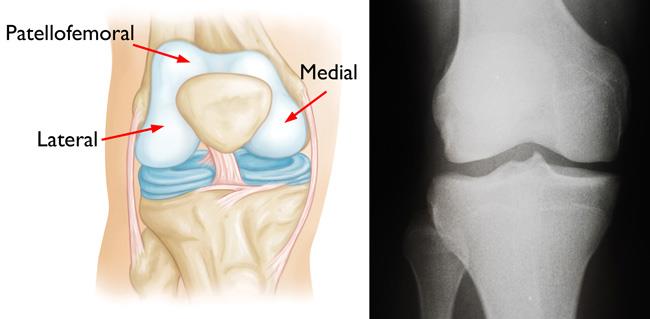
In knee osteoarthritis, the cartilage protecting the bones of the knee slowly wears away. This can occur throughout the knee joint or just in a single area of the knee.
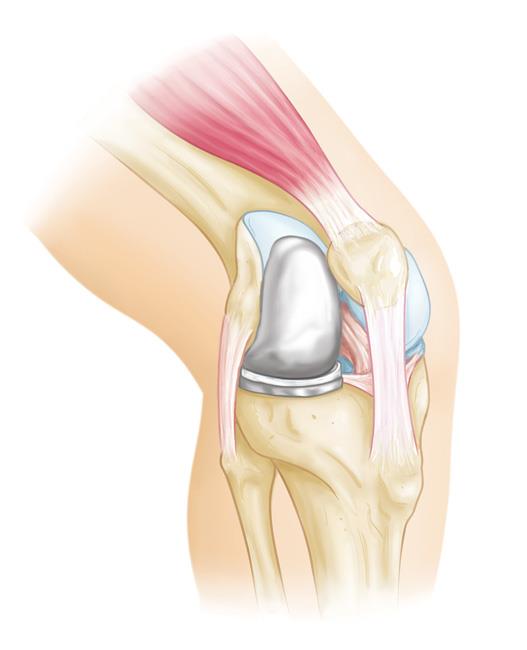
The knee is divided into three major compartments:
- Medial compartment (the inside part of the knee)
- Lateral compartment (the outside part of the knee)
- Patellofemoral compartment (the front of the knee between the kneecap and thighbone)
Advanced osteoarthritis that is limited to a single compartment may be treated with a unicompartmental knee replacement. During this procedure, the damaged compartment is replaced with metal and plastic. The healthy cartilage and bone, as well as all of the ligaments, are preserved.
Advantages and Disadvantages of Partial Knee Replacement
Multiple studies show that most patients who are appropriate candidates for unicompartmental knee replacement have good results with this procedure.
The advantages of partial knee replacement over total knee replacement include:
- Quicker recovery
- Less pain after surgery
- Less blood loss
- Lower risk of infection and blood clots
Also, because the bone, cartilage, and ligaments in the healthy parts of the knee are preserved, many patients report that a unicompartmental knee replacement feels more natural than a total knee replacement. A unicompartmental knee may also bend better.
The disadvantage of partial knee replacement compared with total knee replacement is the potential need for more surgery. For example, a total knee replacement may be necessary in the future if arthritis develops in the parts of the knee that have not been replaced. The need for additional surgery is slightly higher for partial knee replacement than for total knee replacement.
Candidates for Surgery
If your osteoarthritis has advanced and nonsurgical treatment options are no longer relieving your symptoms, your doctor may recommend knee replacement surgery.
To be a candidate for unicompartmental knee replacement, your arthritis must be limited to one compartment of your knee.
If you have any of the following characteristics, you may not be eligible for the procedure:
- Inflammatory arthritis
- Significant knee stiffness
- Ligament damage
With proper patient selection, modern unicompartmental knee replacements have demonstrated excellent medium- and long-term results in both younger and older patients.
Orthopaedic Evaluation
A thorough evaluation by an orthopaedic surgeon will determine whether you are a good candidate for a partial knee replacement.
Medical History
Your doctor will ask you several questions about your general health, your knee pain, and your ability to function.
Location of pain. The doctor will be specifically concerned with the location of your pain. If your pain is located almost entirely on either the inside portion or outside portion of your knee, you may be a candidate for a partial knee replacement. If you have pain throughout your entire knee or pain in the front of your knee (under your kneecap) you may be better qualified for a total knee replacement.
Physical Examination
Your doctor will closely examine your knee. They will try to determine the location of your pain.
Your doctor will also test your knee for range of motion and ligament quality. If your knee is too stiff, or if the ligaments in your knee feel weak or torn, your doctor will probably not recommend unicompartmental knee replacement (although you still may be a candidate for total knee replacement).
Imaging Tests
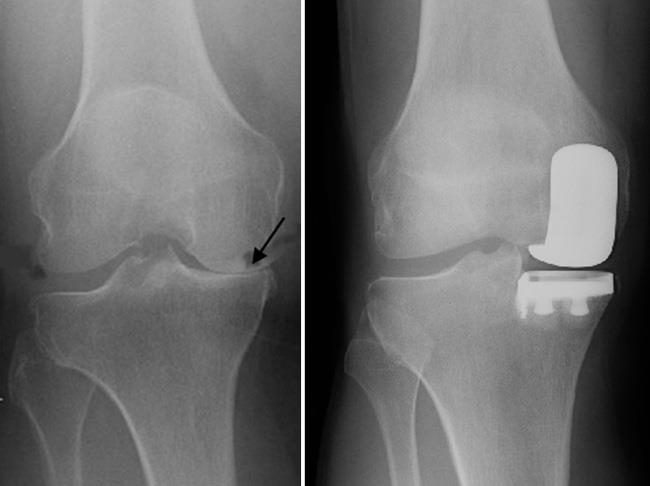
- X-rays. X-rays help to determine the extent of damage and deformity in your knee. Your doctor will order several X-rays of your knee to see the pattern of arthritis.
- Magnetic resonance imaging (MRI) scans. Your doctor may also order an MRI scan to better evaluate the cartilage.
Your Surgery
You will either go home after your surgery or be admitted to the hospital for an overnight stay. Your doctor will discuss the timing with you.
Before Surgery
Before your procedure, a doctor from the anesthesia department will discuss anesthesia choices with you. You should also have discussed anesthesia options with your surgeon during your preoperative clinic visits. Anesthesia options include:
- General anesthesia, in which you are put to sleep.
- Spinal, in which you are awake but your body is numb from the waist down.
- Peripheral nerve block. Nerve blocks are a type of regional anesthesia in which numbing medication is injected near a specific nerve or nerves to block pain sensations from a specific area of the body. These blocks may be used in conjunction with general or spinal anesthesia.
Your surgeon will also see you before surgery and sign your knee with a marker to verify the surgical site.
Surgical Procedure
A partial knee replacement operation typically lasts between 1 and 2 hours.
Inspection of the joint. Your surgeon will make an incision at the front of your knee. They will then explore the three compartments of your knee to verify that the cartilage damage is, in fact, limited to one compartment and that your ligaments are intact.
If your surgeon feels that your knee is unsuitable for a partial knee replacement, they may instead perform a total knee replacement. Your surgeon will have discussed this contingency plan with you before your operation to make sure you agree with this strategy.
Partial knee replacement. There are three basic steps in the procedure:
- Prepare the bone. Your surgeon will use special saws to remove the cartilage from the damaged compartment of your knee.
- Measure the size of your bones and position the metal implants. The surgeon replaces the removed cartilage and bone with metal coverings that recreate the surface of the joint. These metal parts are typically held to the bone with cement. Alternatively, in cementless fixation, the metal parts may be press-fit to the bone to allow bone to grow onto the implant.
- Insert a spacer. The surgeon places a plastic insert between the two metal components to create a smooth gliding surface.
Recovery room. After the surgery, you will be taken to the recovery room, where you will be closely monitored by nurses as you recover from the anesthesia. You will then either be discharged home or taken to your hospital room if you need to stay overnight.
Complications
As with any surgical procedure, there are risks involved with partial knee replacement. Your surgeon will discuss each of the risks with you and will take specific measures to help avoid potential complications.
Although rare, the most common risks include:
- Blood clots. Blood clots in the leg veins are a common complication of knee replacement surgery. Blood clots can form in the deep veins of the legs or pelvis after surgery. Depending on your needs, your doctor may prescribe blood thinners, including oral medications such as aspirin, apixaban (Eliquis), rivaroxaban (Xarelto), or warfarin (Coumadin), or injections such as enoxaparin (Lovenox).
- Infection. After surgery, an infection may occur in the skin over the wound or deep in the wound. Infections can occur days to years after your operation. You will be given antibiotics before the start of your surgery, and these are often continued for about 24 hours after surgery to prevent infection.
- Injury to nerves or vessels. Although it rarely happens, nerves or blood vessels may be injured or stretched during the procedure.
- Continued pain
- Risks of anesthesia
- Need for additional surgery
Recovery
Hospital discharge. Partial knee replacement patients usually experience less postoperative pain and swelling, and have an easier rehabilitation than patients undergoing total knee replacement. In rare cases, patients go to a skilled nursing (rehabilitation) facility after the operation.
Pain management. After surgery, you will feel some pain, but your surgeon and nurses will make every effort to help you feel as comfortable as possible.
Many types of medicines are available to help control pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Treating pain with medication can help you feel more comfortable, which will help your body heal and recover from surgery faster.
Opioids can provide excellent pain relief; however, they are a narcotic and can be addictive. It is important to use opioids only as directed by your doctor and stop taking these medications as soon as your pain starts to improve.
Weightbearing. You will begin putting weight on your knee immediately after surgery. You may need a walker, cane, or crutches for the first several days or weeks until you become comfortable enough to walk without assistance.
Rehabilitation exercise. A physical therapist will give you exercises to help maintain your range of motion and restore your strength.
Doctor visits. You will continue to see your orthopaedic surgeon for follow-up visits in their clinic at regular intervals.
You will most likely be able to resume all of your regular activities of daily living by 6 weeks after surgery.
Get tips on preparing your home for your unicompartmental knee replacement in this infographic (click on image for full infographic).
To assist doctors in the surgical management of osteoarthritis of the knee, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Surgical Management of Osteoarthritis of the Knee - Clinical Practice Guideline (CPG) | American Academy of Orthopaedic Surgeons (aaos.org)
Last Reviewed
September 2021
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.