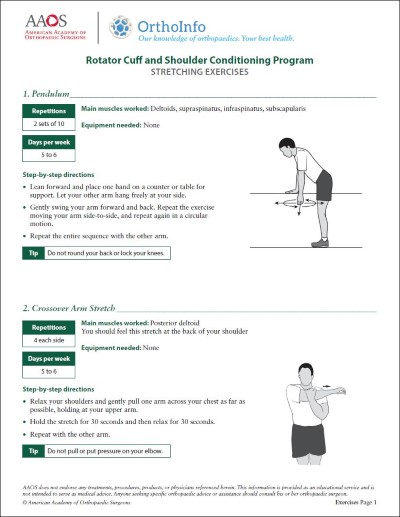
Diseases & Conditions
Biceps Tendon Tear at the Shoulder
Tendons attach muscles to bones. The biceps tendons attach the biceps muscle to bones in the shoulder and elbow. If you tear the biceps tendon at the shoulder, you may lose some strength in your arm and have pain when you forcefully turn your arm from palm down to palm up.
Most people need only simple treatments to relieve symptoms and can still function at a high level with a biceps tendon tear around the shoulder. This is because there are two attachments of the biceps tendon in the shoulder and typically, a tear only involves one.
You may benefit from surgery to repair the torn tendon if:
- Your symptoms cannot be relieved by nonsurgical treatments
- You develop debilitating (unbearable) cramping in the biceps muscle
- You develop significant shoulder pain
- Your arm weakness prevents you from working or performing daily activities, such as bathing, getting dressed, cooking, cleaning, or shopping
Anatomy
The shoulder is a ball-and-socket joint made up of three bones:
- The upper humerus (upper arm bone)
- The scapula (shoulder blade)
- The clavicle (collarbone)
The head, or ball, of the upper arm (humerus) bone fits into a rounded socket in the shoulder blade. This socket is called the glenoid. A combination of muscles and tendons keeps the ball centered in the shoulder socket. These tissues, called the rotator cuff, cover the ball and attach it to the shoulder blade.
The upper end of the biceps muscle has two tendons that attach it to bones in the shoulder called the long head and the short head:
- The long head attaches to the top of the shoulder socket (glenoid).
- The short head attaches to a bump on the shoulder blade called the coracoid process.
Description
Biceps tendon tears can be either partial or complete.
- Partial tears. The tear does not completely detach the tendon from the bone, and some portion of the tendon is still intact (whole).
- Complete tears. The tear completely detaches the tendon from the bone, and the tendon is no longer intact.
In many cases, torn tendons begin by wearing down or fraying (becoming ragged). As the damage progresses, the worn tendon can completely tear, sometimes when you are lifting a heavy object.
The long head of the biceps tendon is more at risk of being injured. This is because it travels through the shoulder joint to its attachment point in the socket.
Fortunately, the biceps has two attachments at the shoulder. The short head, or second attachment, of the biceps rarely tears. Because of this second attachment, most people can still use their biceps muscle even after a complete tear of the long head.
When you tear your biceps tendon, you can also damage other parts of your shoulder, such as the rotator cuff tendons.
Cause
There are two main causes of biceps tendon tears: injury and overuse.
Injury
If you fall hard on an outstretched arm or lift something too heavy, you can tear your biceps tendon.
Overuse
Many tears are the result of wearing down and fraying of the tendon that occurs slowly over time. This is more common than a tear from an injury and naturally occurs as we age. It can be worsened by overuse — repeating the same shoulder motions again and again.
Overuse can cause a range of shoulder problems, including tendinitis, bursitis, shoulder impingement, and rotator cuff injuries. Having any of these conditions puts more stress on the biceps tendon, making it more likely to weaken or tear.
Risk Factors
Your risk for a tendon tear increases with:
- Age. Older people have put more years of wear and tear on their tendons than younger people.
- Heavy overhead activities. Too much weight during weightlifting or overload activities is a risk, and many jobs that require heavy overhead lifting can create excess wear and tear on the tendons.
- Shoulder overuse. Repetitive overhead sports, such as swimming or tennis, can cause more tendon wear and tear.
- Smoking. Nicotine use can weaken tendons.
- Corticosteroid medications. Using corticosteroids can lead to increased muscle and tendon weakness.
Symptoms
- Sudden, sharp pain in the upper arm.
- Sometimes an audible pop or snap.
- Cramping of the biceps muscle with strenuous use of the arm.
- Bruising of the upper arm down toward the elbow.
- Pain or tenderness at the shoulder and the elbow.
- Weakness in the shoulder and the elbow.
- Difficulty turning the hand palm up or palm down.
- "Popeye muscle," or "Popeye deformity." Because a torn tendon can no longer keep the biceps muscle tight, you may see a bulge in the upper arm above the elbow, with the muscle appearing closer to the elbow than it does on your other arm (see photo below).
Doctor Examination
Medical History and Physical Examination
After discussing your symptoms and medical history, your doctor will examine your shoulder. The diagnosis is often obvious for complete tears because of the deformity of the arm muscle ("Popeye Muscle" or "Popeye deformity").
Partial tears are less obvious. To diagnose a partial tear, your doctor may ask you to bend your arm and tighten the biceps muscle. Pain when you use your biceps muscle may mean there is a partial tear.
It is also very important that your doctor identifies any other shoulder problems when planning your treatment, so they may order additional tests. Rotator cuff injuries, impingement, bursitis, and tendinitis are some conditions that you may have in addition to a biceps tendon tear.
The biceps can also tear near the elbow, although this is less common. A tear near the elbow will cause a gap in the front of the elbow and is more likely to require surgery than a tear near the shoulder. Your doctor will check your arm for damage to this area.
Imaging Tests
- X-rays. Although X-rays cannot show soft tissues like the biceps tendon, they can be useful to look for other problems that can cause shoulder and elbow pain.
- Ultrasound. An ultrasound may help evaluate the soft tissues of the shoulder. This is typically a simple test; however, the usefulness of the ultrasound depends a great deal on the expertise of the provider performing the test.
- Magnetic resonance imaging (MRI). MRI scans create better images of soft tissues than X-rays. They can show both partial and complete tears.
Treatment
Nonsurgical Treatment
For most people, pain from a biceps tendon tear goes away over time. Mild arm weakness or arm muscle deformity do not typically bother most patients, and patients are able to return to their activities and jobs without limitations.
In addition, if you have not damaged a more critical structure, such as the rotator cuff, nonsurgical treatment is a reasonable option. This can include:
- Ice. Apply cold packs for 20 minutes at a time, several times a day to keep down swelling. Do not apply ice directly to the skin.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs like ibuprofen, aspirin, or naproxen can reduce pain and swelling.
- Rest. To relieve pain and limit swelling, avoid heavy lifting and overhead activities. Your doctor may recommend using a sling for a brief time.
- Physical therapy. Flexibility and strengthening exercises will restore movement and strengthen your shoulder.
Surgical Treatment
You rarely need surgical treatment for a long head of the biceps tendon tear. However, some people may benefit from surgery, including:
- Those who develop severe cramping of the muscle
- Those who develop significant shoulder pain
- Those who require complete recovery of strength, such as athletes or manual laborers
- Those with partial tears whose symptoms are not improved with nonsurgical treatment
Procedure. Several procedures have been developed to repair the tendon with minimal incisions.
- The goal of the surgery is to attach the torn tendon back to the shoulder.
- It is uncommon to re-attach the torn tendon to the top of the socket (glenoid); rather, it is often reattached to the arm bone (humerus).
- Your doctor will discuss with you the options that are best for your specific case.
Complications. Complications with this surgery are rare. Re-tearing of the repaired tendon is uncommon.
Rehabilitation. After surgery, you may be required to wear a sling for a brief period of time to keep your shoulder from moving.
Your doctor will soon start you on physical therapy exercises.
- Flexibility exercises will improve the range of motion in your shoulder.
- Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan.
Be sure to follow the treatment plan given to you by your doctor. Although rehabilitation is a slow process, your commitment to physical therapy is the most important factor in eventually returning to all the activities you enjoy.
Surgical Outcome. Successful surgery may correct muscle deformity and improve your arm's strength and function.
Last Reviewed
May 2024
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.